What’s the difference between an epidemic and an endemic disease? And what does it mean when an epidemic is reclassified as endemic? The answers to these questions lie in epidemiology, the systematic, data-driven study of health and disease in populations. But as historian Jacob Steere-Williams reveals, this most scientific of fields emerged in the 19th century imbued with a doctrine of Western imperialism – a legacy that continues to influence how we talk about disease.
Epidemic threats and racist legacies
Words by Jacob Steere-Williamsartwork by Dark Matteraverage reading time 7 minutes
- Article

Doctors have always been interested in the origins and spread of disease. From antiquity to the modern age, diseases have been attributed to a vast number of overlapping causes, from religious deities and the moral character of an individual to the environment and the cosmos.
With growing urban populations and increasing global travel, 19th-century medicine was focused on both the persistence of diseases such as typhoid in large communities (endemic diseases) and the global spread of diseases such as cholera (epidemics). But when the modern science of epidemiology began in the mid-19th century, the scientific study of disease was imbued with a Western imperialist doctrine of blame, and moral decay on a global scale.
In his landmark study of 1862, ‘A Treatise on the Continued Fevers of Great Britain’, Charles Murchison declared typhoid fever “the endemic fever of England”. Using patient admissions to the London Fever Hospital, where he served as physician, Murchison argued that what made typhoid (also known as pythogenic fever) endemic to England was that it was always present. Typhoid and typhus have similar symptoms but different origins and behaviour. Whereas cases of typhus fever fluctuated from year to year, typhoid was rooted in the population and place.
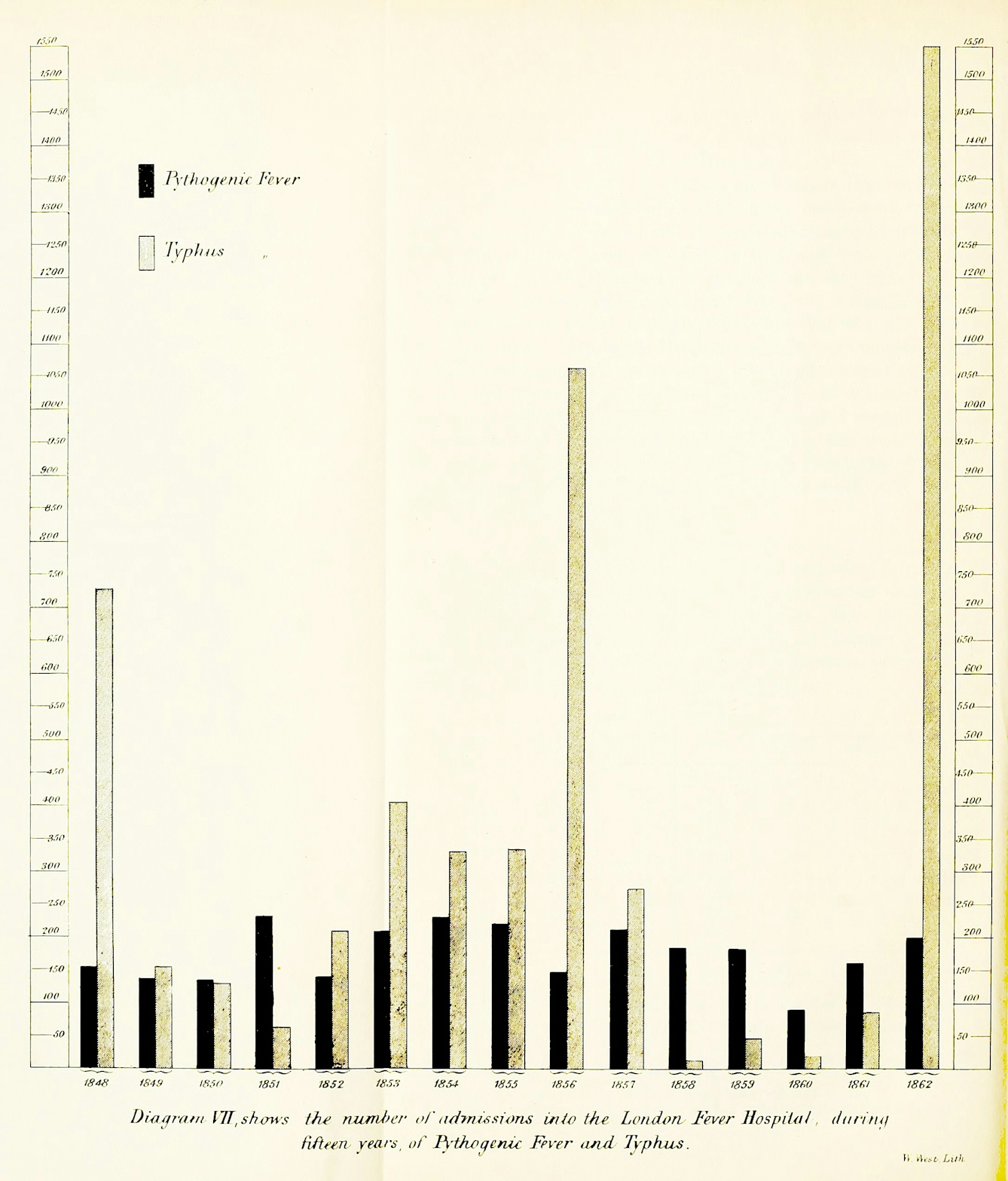
A table from Murchison’s book indicating the endemic nature of typhoid (pythogenic fever), which is always present at a steady rate in the population, and the epidemic nature of typhus, which arises and recedes in distinct outbreaks.
By the time of Murchison’s study, Western physicians were using the term ‘endemic’ to describe diseases that regularly occurred in specific locations. Derived from the Greek words for ‘in’ and ‘people’, endemic was tied to location in the ‘Airs, Waters, Places’ doctrine of classical Western medicine. This doctrine held that the physical and mental health of an individual was intimately tied to place, including climate, weather, food, water and season.
From endemic to epidemic and back again
The term endemic was yoked to another, more familiar term, epidemic, which in the 19th century referred to an imported and often contagious disease. But endemic and epidemic were relational terms: some endemic disease might become epidemic, and some epidemic diseases might revert back to being endemic.
The classic disease used for thinking about the fluctuations of endemic and epidemic was malaria. Henry Stephens, member of the Royal College of Surgeons, in 1849 went as far as to use ‘malarious’ as a synonym for endemic diseases, noting that they are “ordinarily the disease of a district, having a local origin and local habitation”. “Yet occasionally,” Stephens said, “they will assume the march and character of an epidemic.”
Framing cholera’s origin as endemic to India was part of an imperialist doctrine of blame at the heart of global health... one with legacies that continue today.
The study of the relationship between endemic and epidemic, and the complex reasons why some endemic diseases erupted as epidemics, was at the centre of the rise of the modern field of epidemiology and global thinking about disease. As John Macpherson, Inspector-General of Hospitals in Bengal in colonial India, noted in his book 'The early seats of cholera in India', “No question in medicine is more interesting than that of an endemic disease taking on the character of an epidemic, and of the behaviour of an endemic, when its own epidemic form reaches it.”
Epidemiology and Western imperialism
Entangled with the rise of modern epidemiology was the global march of Western imperialism and colonisation, which reframed epidemics as not just contagious and non-localised but foreign and aggressive. Diseases framed as endemic to Europe, like typhoid, were easier to explain through the ‘Airs, Waters, Places’ doctrine. But diseases such as cholera and plague, understood to be endemic to the Middle East and Asia, apparently required a different kind of logic.
Framing cholera’s origin as endemic to India, for example, was part of an imperialist doctrine of blame at the heart of global health, with racist presumptions, one with legacies that continue today. British doctors like Ernst Hart, long-time editor of the British Medical Journal, declared that cholera was “a filth disease” of India, “carried by dirty people to dirty places, and there spread by dirt and the use of dirty water”.

John Bull, the personification of England, captures cholera, personified as Asiatic, trying to enter Britain. The disease was endemic across Asia, and 19th-century cholera epidemics in Britain were presumed to originate in India, the UK’s key Asian colony.
Endemicity in the colonies was used by Western doctors as a value judgement in diseases, like cholera, “of the inferior social and hygienic”, “moral influences, and irregularities of life” among “the natives of India”, John Sullivan of the Royal College of Physicians opined in 1877.
Epidemics of cholera or plague that struck Europe might be, as Henry Stephens noted in 1849, an “invading army”, that brought with them not just pestilential terror, but the threat of moral decay, which is why pandemics and xenophobia are almost inextricably bound together.
Mapping disease on the “highways of man”
When a disease like cholera erupted into an epidemic, it followed, Sullivan noted in 1877, “the direction of the highways of man”. From the second half of the 19th century, doctors attempted to map and visualise the global patterns of endemicity and epidemicity. The Scottish geographer Alexander Keith Johnston, a corresponding member of the Epidemiological Society of London, produced in 1856 ‘The Geographical Distribution of Health & Disease’, a colour-coded map that attempted to situate the origins of diseases and their spread as epidemics.
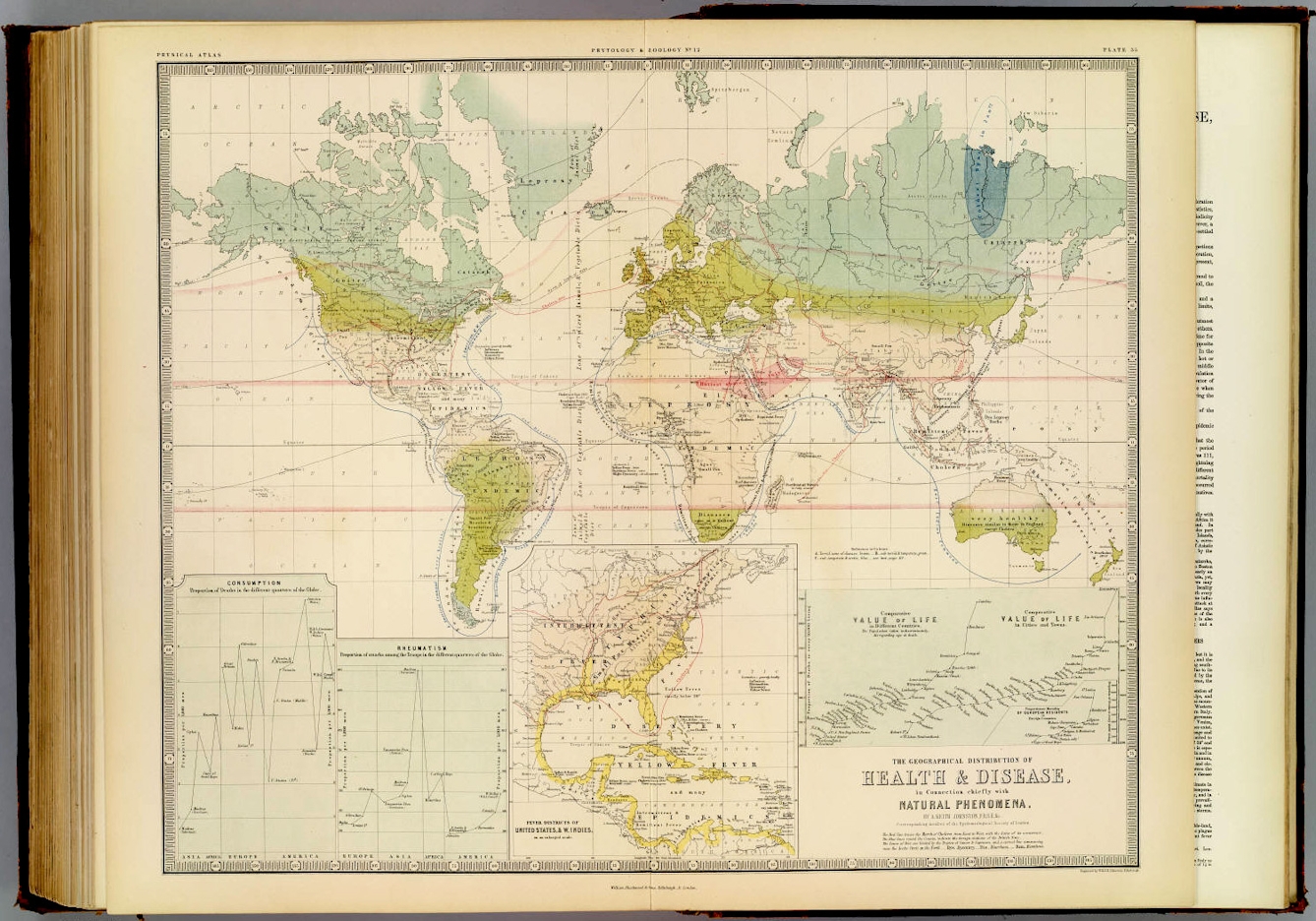
Epidemiological mapping of diseases on a global scale such as Johnston’s ‘Geographical Distribution of Health & Disease’ showed the ‘foreign’ sources of epidemics in Europe and North America and locations that were ‘healthy’ for Europeans.
Johnston’s map connected yellow-fever epidemics from Philadelphia to Haiti to Cartagena. Leprosy, in this visualisation, was endemic to South America, parts of Africa, and India. Cholera was endemic to India, and typhus to Europe. And the moral and racial influence of epidemiological thinking was at the core of Johnston’s map. Colonised Southern Africa and Australia, for example, were explained as “very healthy”, and “diseases same as in England except cholera”.
Interestingly, Johnston’s map also attempted to visualise the geographical pathways whereby endemic diseases spread in epidemic patterns. He used red lines, for instance, to show the march of cholera in 1832 and 1848, and arrows to show where cholera came from and how it reached the West.
Global health in a post-colonial age
The fluidity between the endemic and epidemic began to change from the late 19th century, both with more reductionist, biomedical understandings of disease, and with major shifts in the global distribution of infectious disease. Endemic continued to mean diseases of specific locations and to many in the Global North endemicity also came to mean remote diseases that were a low-level threat, easily contained.
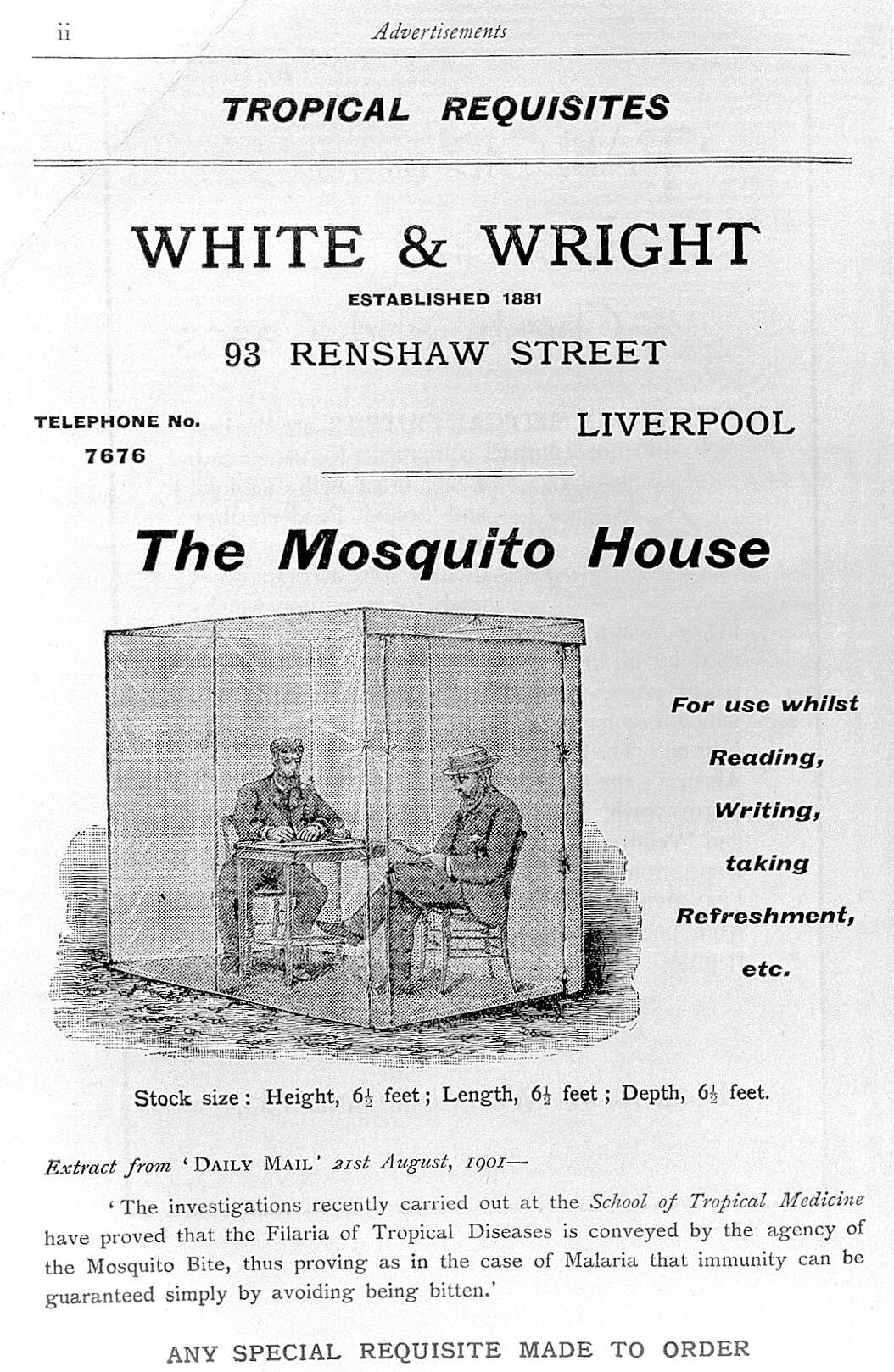
Mosquito netting advertised in 1902 to Westerners living and working in (colonial) countries where malaria was endemic. It allowed them to go about their business safe in the knowledge that "immunity can be guaranteed simply by avoiding being bitten".
Thus malaria, classed as endemic in much of the Global South, continued to kill millions but, because it was not an epidemic threat and could be contained, did not warrant significant medical and research resources on a global scale. Increasingly, experts in the Global North came to disregard many previous disease threats like cholera, typhoid and plague, which seemingly ‘disappeared’ in the Global North but remained ‘endemic’ in the Global South. In other words, the politics of the post-colonial world masked the way in which endemicity had been tied to colonialism.
Signalling the end of the Covid-19 pandemic
The legacy of the endemic and epidemic diseases remains with us. In early 2022, as the mass vaccination programme across the Global North began to take effect and mortality rates fell, there was a push in western Europe and North America to recategorise Covid-19 as endemic, signalling a subtle shift in how it should be perceived.
The disease was no longer a significant global threat, but something generally mild and inevitable. It may still be spreading in epidemic proportions in other parts of the world with lower vaccination levels, but for the Global North the change in perception signalled that the pandemic was coming to an end.
As 19th-century epidemiologist Gavin Milroy quipped in 1870, “The general subject of epidemiology is indubitably mysterious and complex,” but it is not without politics.
Read more
About the contributors
Jacob Steere-Williams
Jacob Steere-Williams is an historian of epidemic disease, particularly in 19th- and early 20th-century Britain and the former British colonies. He is the author of the book ‘The Filth Disease: Typhoid Fever and the Practices of Epidemiology in Victorian England’ (2020) and Associate Professor of History at the College of Charleston.
Dark Matter
Dark Matter is the pseudonym of illustrator, animator and artist Chris Arran. He creates animated collages that are fizzing and sparkling with style, blending live-action footage with animation, 3D, illustration and sharp editing. His art is defined by his curiosity, exploring a variety of ideas, including the beauty of black skin, the celebration of age, and questions about sustainability and ways to live in a more vibrant world. His works are driven by the universal energy that connects us all, exuding positivity and giving a voice to inclusivity and diversity.

