In 1846 a Vienna hospital saw hundreds of new mothers die of postpartum infections. A young member of staff, Hungarian doctor Ignaz Semmelweis, soon worked out why. But he needed inhuman strength to battle the establishment. Find out how he made his groundbreaking discovery and fought to institute new practices, and how we still benefit in our daily lives.

More than 170 years before government campaigns such as “hands, face, space” became a tactic to combat coronavirus, one man was already advocating handwashing to prevent the spread of disease. Hungarian physician Ignaz Semmelweis had made the huge discovery that childbed fever – the name given to an infection of any part of the reproductive tract after giving birth – could be eradicated by sanitary practices, but found himself being ignored, sidelined and then forced to live in an asylum, where he died ignominiously.
Semmelweis should have been lauded as a hero, but instead his story is about the price people sometimes have to pay to be on the right side of history. Today his legacy lives on, not only in disease prevention, but in the solemn lesson that ignoring dissenting scientific voices can cause millions of preventable deaths.
It was very common for doctors to examine bodies in what was known as the “dead house” and then immediately assess pregnant women.
His tale is, in fact, so entrancing that it was set to be told in a play, until the production was postponed after the coronavirus pandemic caused theatres to close. The cruel irony of Semmelweis’s words being silenced in the 21st century is a leitmotif for the man who faced a tragic battle against snobbery, xenophobia and vested interests.
The pioneering Hungarian was, though, a complex character in a complex time. He spoke German, but was a Hungarian nationalist at a time when the Austrian Empire, which included Hungary, cracked down on academic dissent. He had a brilliant mind, but was prone to mood swings, to the point where some have claimed he was bipolar. And he was obsessive, discourteous and undiplomatic, leading him to gain far more enemies than followers.
“He was brilliant, though,” says Stephen Brown, who wrote the play ‘Semmelweis’, which had been due to open at the Bristol Old Vic in summer 2020. “He was not, perhaps, quite in the league of Louis Pasteur. But to make the series of deductions and theories of reasonings that he did was very brilliant.”
A gruesome realisation
At the age of 28, in 1846, Semmelweis was made assistant of the first division (obstetrics) of the Vienna General Hospital under Professor Johann Klein, who had overseen a rise in the death rate from childbed fever from 1 per cent to 7.45 per cent. Under Klein “policies were conservative and opposition was stifled”, according to Sherwin Nuland’s 2004 book about Semmelweis, ‘The Doctors’ Plague’.
In that year the division recorded 459 deaths to postpartum mothers, but other wards, where midwives assisted labour, recorded far lower fatalities from the disease. Some months, in the division Semmelweis worked in, as many as 30 per cent of postpartum mothers died of childbed fever. There was also a lower mortality for births undertaken at home, or even in alleyways. Epidemics were always hospital-based and invariably worse in the obstetrics division.
At the time Vienna General was one of the leading hospitals in Europe, attracting medical students from all over Europe, who were especially drawn to its renowned autopsy experiments. It was very common for doctors to examine bodies in what was known as the “dead house” and then immediately assess pregnant women.

“Although he didn’t make the connection with germs... Semmelweis placed a solution of calcium hypochlorite at the entrance of the first division, insisting every medical attendant wash their hands before touching a woman in labour.”
Semmelweis noticed that mortality rates in the obstetrics division were a lot higher than in the midwife-led wards and would decrease seasonally, particularly outside the students’ term times. But his discovery was only realised after the death of his friend Jakob Kolletschka, Professor of Forensic Medicine, in 1847. Kolletschka died after accidentally being poked by a student’s scalpel, and an autopsy Semmelweis conducted revealed that his body contained a pathogen similar to one causing childbed fever.
Putting theory into practice
Although he didn’t make the connection with germs, like Pasteur did later, Semmelweis thought cadaver particles were the cause, and placed a solution of calcium hypochlorite at the entrance of the first division, insisting every medical attendant wash their hands before touching a woman in labour.
The results were extraordinary: in the last seven months of 1847 only 56 women died out of the 1,841 who delivered. Semmelweis’s simple measure had caused the death rate to plummet; it was now comparable to that of those women being seen by midwives.
However, having handwashing adopted as common practice proved problematic, as doctors were opposed to an untested theory that would attribute thousands of deaths to their hands.
“People find it hard to throw away their old theories,” Brown says. “It becomes very hard to abandon them because you sort of abandon your whole world view. You can very easily look at these medics in the 19th century and call them ‘bloody idiots’. But the understanding of illness then did not fundamentally exist. It required them to acknowledge that they had killed very many people.”
A dissenter in exile
The following year saw the 1848 uprisings, when nations sought to break free of the empire. In Austria this caused a suspicion of new ideas, particularly from Hungarians, and Semmelweis found himself in exile after his assistantship was not renewed. At the same time, one of his more ardent supporters, obstetrician Gustav Adolf Michaelis, killed himself over the guilt he experienced after the death of his cousin, whom he examined several days after she gave birth.

“His family tricked him into being committed to what was then called a lunatic asylum, and he was killed, aged 47, after being beaten by several guards.”
Semmelweis returned to Hungary and worked in Budapest’s Szent Rókus Hospital, where he faced regular battles over hygiene standards, despite eradicating the cases of childbed fever. During this period nurses circumvented his rules as he went to war with parsimonious bureaucrats over dirty bed linen, famously throwing soiled sheets onto one administrator’s desk.
Worse still, it took him until 1861 to actually write down his theory on handwashing, and when he did, it was more than 550 pages long, virtually unreadable and self-glorifying.
“He was watching this awful thing happening,” adds Brown, about the many deaths that could have been prevented by hand hygiene. “It just seems to have lodged very deep in his heart and he couldn’t cope with it.”
Descent into chaos
After his theory was ridiculed, Semmelweis started experiencing a type of depression and had various antisocial outbursts, including writing letters to prominent physicians accusing them of being “partners in a massacre”. He started drinking heavily and began an extramarital affair with a prostitute.
His family tricked him into being committed to what was then called a lunatic asylum, and he was killed, aged 47, after being beaten by several guards. The autopsy in 1865 said he had died of sepsis, the very disease he did so much to prevent.

“It’s easy today to take handwashing for granted, but it’s because of the hard work and sacrifices made by Semmelweis and others that we have the knowledge to stop the spread of deadly viruses.”
Two years after Semmelweis’s death, Scottish surgeon Joseph Lister began promoting handwashing and sanitising surgical equipment. Although his ideas also met with fierce criticism, physicians in the 1870s began scrubbing up before and after operations. Two decades later, Louis Pasteur recognised Semmelweis’s work and provided the definitive evidence on germ theory and antiseptic techniques.
“Very powerfully, coronavirus has actually made us aware,” adds Brown, “of the fact that, as it has been for 150 years, hand hygiene is a fundamental part of basic disease prevention.”
It’s easy today to take handwashing for granted, but it’s because of the hard work and sacrifices made by Semmelweis and others that we have the knowledge to stop the spread of deadly viruses, such as the one that causes Covid-19.
Semmelweis may not have discovered germs, but he discovered the way to kill them, and the results of his dogged investigations have saved countless lives. He also is an inspiration to those in medicine who have gone against the establishment, and a stark warning of the great personal cost such dissent involves.
About the contributors
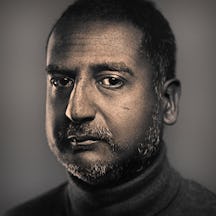
David Jesudason
David Jesudason is a freelance journalist who covers race issues for BBC Culture, Pellicle and Vittles. He was named Beer Writer of the Year in 2023, after his first book ‘Desi Pubs, A Guide to British-Indian Pubs, Food and Culture’ was hailed as “the most important volume on pubs in 50 years”. David also writes ‘Pub Episodes of My Life’, a weekly newsletter about the drinking establishments that serve marginalised people.
Steven Pocock
Steven is a photographer at Wellcome. His photography takes inspiration from the museum’s rich and varied collections. He enjoys collaborating on creative projects and taking them to imaginative places.