The EEG (electroencephalograph) literally electrified the diagnosis and treatment of epilepsy. Aparna Nair recalls the dreaded EEG tests of her adolescence and discovers that the technology was also used to define and reject people with epilepsy.
Electrical epilepsy and the EEG Test
Words by Aparna Nairartwork by Tracy Satchwillaverage reading time 6 minutes
- Serial

The discovery of electrical activity in the brain and nervous system gave physicians a new way to investigate the brain. They looked for ways to measure and record the tiny electrical currents emitted from deep inside the head.
In the early 20th century, the electroencephalograph (EEG) was developed to produce graphical representations of electrical ‘brain waves’ that could be studied and compared to identify the characteristics of conditions such as epilepsy. The technology soon became an essential part of the diagnosis and monitoring of seizures and epilepsy.
The dreaded EEG test
Visiting the hospital for an EEG appointment was a frequent, much-feared event of my adolescence. Accompanied by my mother, I visited a big, sprawling hospital in the heart of the South Indian city where we lived. My mother was so nervous I could feel the fear and anxiety radiating off her skin and settling into my bones. I tried to be unemotional for her, but I am not sure I was ever successful.

Aparna Nair with her mother.
The hospital always bustled with people and seemed to simmer in the heat and humidity. But the EEG machine took pride of place in a dark, cave-like room, which was always briskly cold and sterile. The technician who operated the device was a stern woman whose face I still remember. She rarely smiled, and then usually at my mother.
As she sat me down and shook my long, curly hair out of its customary braids, my stomach clenched in anticipation of what was to come. Then she cleaned my scalp with spirit and used the fingernail of her index finger to rub a mud-coloured clay into my head. It always brought tears to my eyes and occasionally spots of blood would seep out onto my skin, especially when she reached the tender areas above my ears.
After the clay paste came the electrodes, which were attached to my scalp, forming a bizarre kind of plastic-and-wire frame for my head. As I lay down on the white-sheeted gurney I could feel my heart pounding in my chest and my pulse throbbing in my temples in sick anticipation of the impending aura – the rising change of perceptions and sensations that always precedes a seizure for me.

A woman wired up for an EEG test in 2012. The results are displayed on the monitor.
The technician would ask me to try to relax, then ask me to perform a few basic tasks. Next she positioned a large round lamp in front of me, which flashed pulses of light into my cringing face. The lights started off flashing slowly, then progressively faster, and my brain started screaming as an aura was triggered.
The light was used to assess my photosensitivity and whether or not flashing lights could trigger seizures. The ‘evidence’ of my photosensitivity and epilepsy was recorded as an inked geometric scrawl of brainwaves printed on thin pink graph paper: a map of the electrical earthquakes in my brain and decipherable only by my doctors. I hated the EEG as a teenager, and now, as an adult, I still have EEG tests to monitor my condition and nothing has changed.
The invention of the EEG
The electroencephalograph (EEG) was invented by the German psychiatrist and researcher Hans Berger (1873–1941). In 1929 he discovered that the brain’s electrical activity and output could be measured and subsequently categorised. His early model of the EEG used platinum needles inserted into the scalp to detect the electrical currents; the needles were later replaced by small metal discs (electrodes) placed on the scalp.
The EEG established that the electrical activity of the brain varied during sleep, waking, seizures and anaesthesia. In 1932, Berger published a report showing the progressive brainwave changes during a seizure lasting 11 minutes. The use of EEG in the diagnosis of epilepsy increased rapidly once Berger’s work was confirmed, to become the definitive diagnostic test for epilepsy.
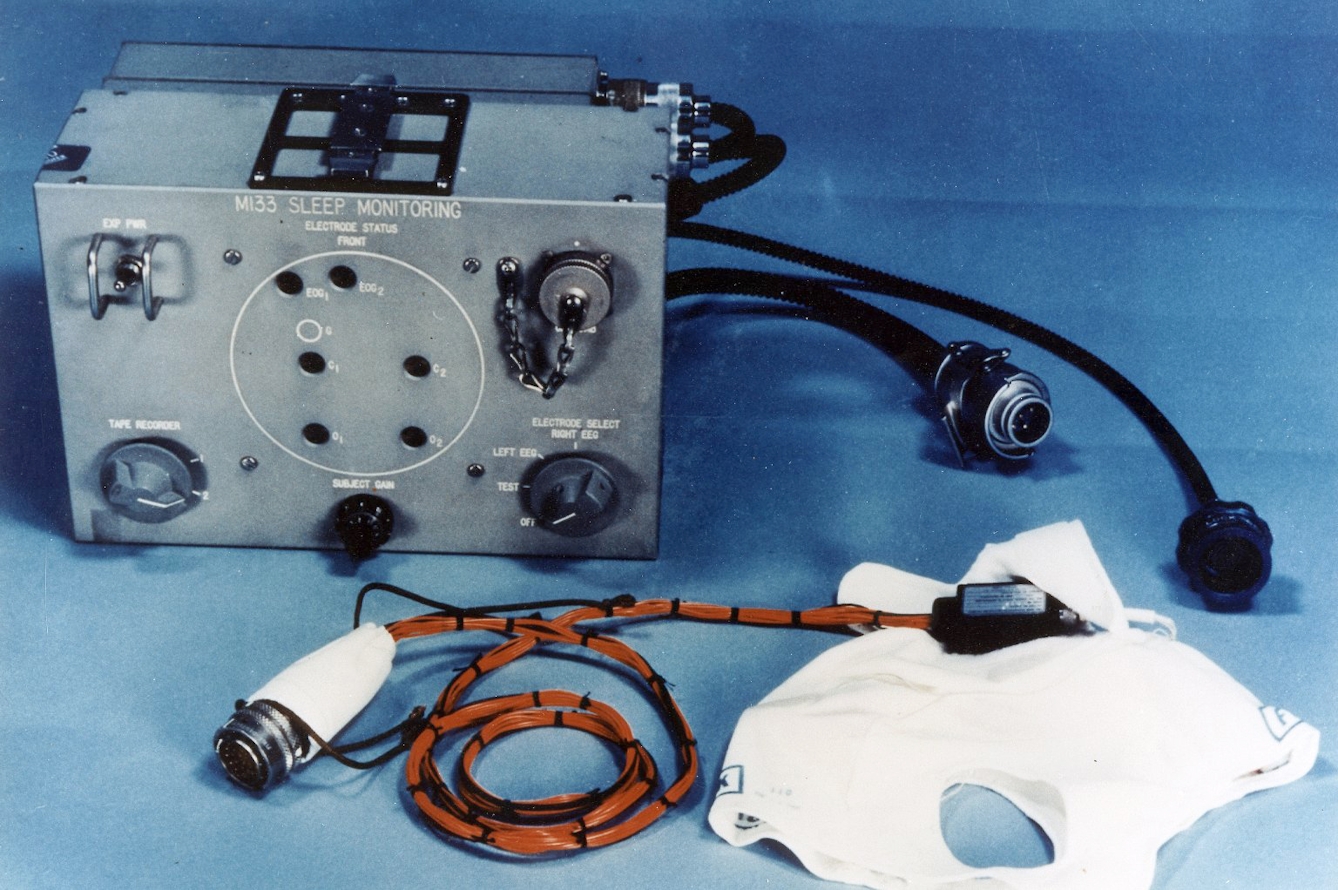
Equipment used to monitor and record EEG and electro-oculographic (EOG) activity during astronauts’ sleep. NASA, 1970.
The EEG came into its own as a general-purpose diagnostic tool in World War II. For the substantial number of troops with head injuries, the EEG was used to locate and identify the extent of brain damage. It also proved useful in tracking the effectiveness of treatment. Seizures and trauma-related epilepsy was often reported among veterans, and the EEG was a regular feature in their diagnosis and care.
By the end of World War II, the use of the EEG had spread across the world and by the end of the 1940s, most major hospitals in the global north recognised its value.
The stigma revealed by brainwaves
Non-medical applications for the EEG were soon found, chiefly as a way to assess the ‘quality’ of human beings. It was used as part of the procedure to select pilots for the air force, and military services around the world used it to screen out “neuropsychiatrically unfit recruits”, those” judged more likely to develop psychological disorders under war conditions. This included the “dangerous epileptic”.
Some scientists set out to see if they could establish characteristic brainwave patterns for populations that they believed might be ‘wired differently’. Groups subject to these kinds of tests included criminals, ‘delinquents’ and inmates of asylums, as well as ‘normal’ men and women. The EEG filtered into public consciousness as a technology to identify hidden ‘weaknesses’ in society. Newspapers in the United States suggested that couples could exchange printouts from the ‘brain-wave writer’ to ensure that neither of them carried the ‘taint’ of epilepsy.
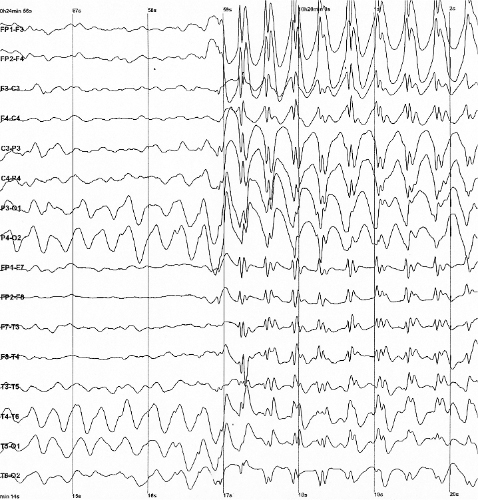
The output of an EEG test showing generalised spike and wave discharges in a child with childhood absence epilepsy (characterised by brief staring spells during which the child is not aware or responsive).
EEG readings were also used in courts on both sides of the Atlantic. Notoriously, the machine was featured in the trial of Jack Ruby, the killer of Lee Harvey Oswald, who had assassinated US President John F Kennedy in 1963. The expert witness for the defence was neurologist and EEG pioneer Frederic Gibbs, who testified that Ruby had psychomotor epilepsy because his EEG readings:
“…show[ed] seizure disorders of the psychomotor variant type” and suggested that these subjects manifest personality instability, lack of emotional control and eccentricities in behavior. He further felt that Ruby killed Oswald during a fugue state induced by an attack of psychomotor seizure.
The intention may have been to mitigate Ruby’s actions, but it also reinforced associations between epilepsy and criminality.
The EEG was developed as a tool to study to the function of the living brain, and it did much to improve the diagnosis and treatment of epilepsy. Ironically, the same technology that helped to identify epilepsy was then used to stigmatise and control people with the condition.
For me nothing has changed. I hated the experience of the EEG as a teenager for the ways in which it overstimulated and exhausted my brain. And as an adult, I still dread it, even though I understand why I need to monitor my illness.
About the contributors
Aparna Nair
Dr Aparna Nair is an assistant professor in the Department of History of Science at the University of Oklahoma. She works on disability, medicine and colonialism in India in the 19th and 20th centuries, as well as disability in popular culture and the experience of epilepsy in South India.
Tracy Satchwill
Tracy Satchwill was born in London, grew up in South Wales and is now based in Norfolk. Working across film, collage, photography and installation, her art practice explores female power, reflecting on its removal or reclamation. She weaves personal narratives into her work, exploring identity, oppression and vulnerability to combine the feminine with the surreal, the uncanny and the weird. Satchwill has exhibited at galleries and institutions across the UK and internationally. She also works on public commissions and residencies, focusing on women’s experiences.

