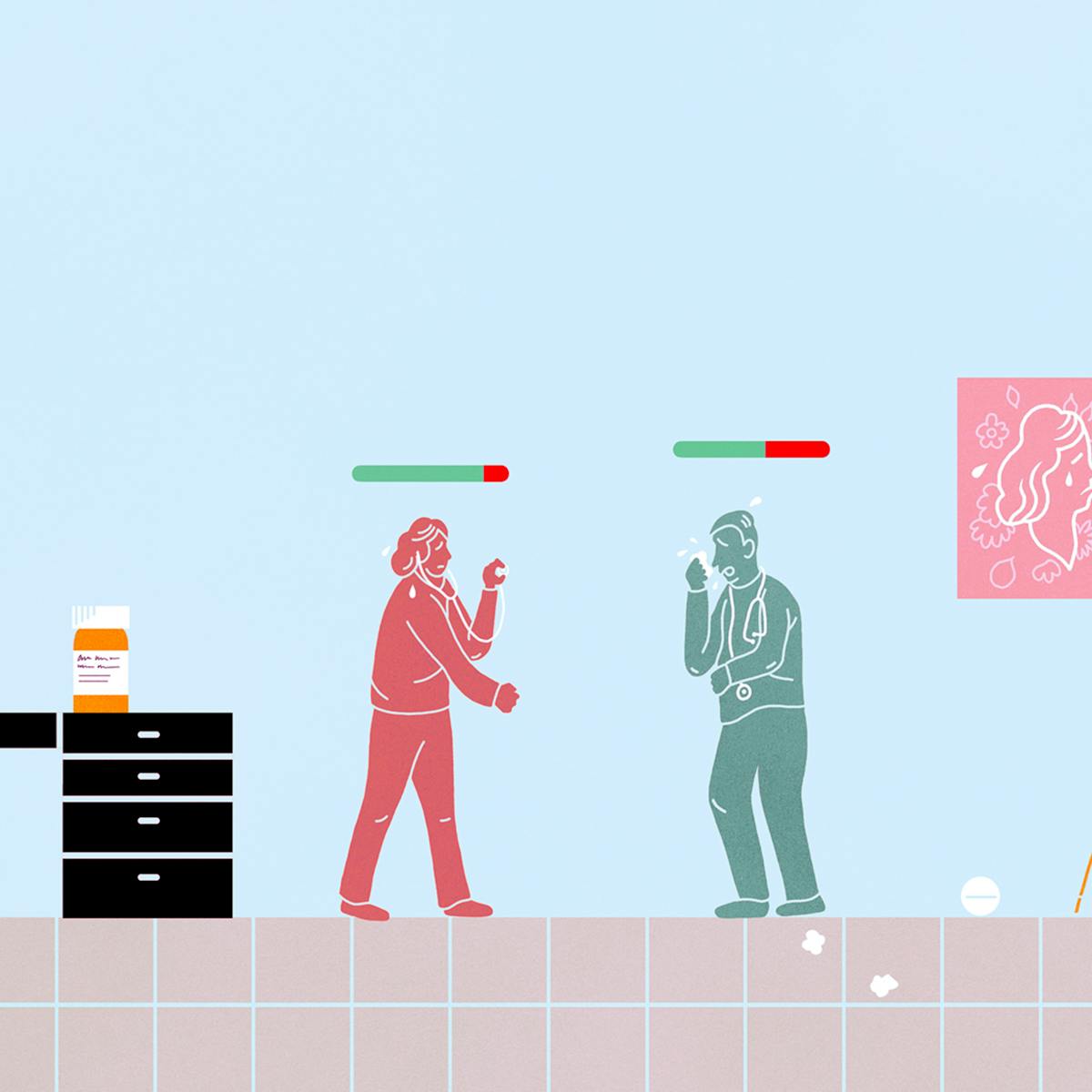
Taking time off for illness creates no end of problems for family doctors. Our anonymous GP presents the case for putting a more supportive system in place.
When doctors get sick
Words by The Secret GPaverage reading time 5 minutes
- Article
I had a minor health complaint this week – an eye problem. As I was at work, I asked a trusted colleague to take a look, and he agreed that it needed further review. Oh no, I thought, it’s a Monday lunchtime and I have a full clinic booked until after 6pm; half of them are urgent appointments – people who had booked that day as they felt their health problems could not wait. I was due to be working the next couple of days too, so when and how could I seek the help I needed?
There were no extra available GPs to cover my clinics, and calling in sick the next day would result in over 30 appointments being cancelled at short notice. I knew that if I had seen a patient with my problem, I would have sent them straight to see a specialist that day.
My colleague was sympathetic, but he is also my boss, so if I had taken the whole afternoon off it would have had a huge impact on him. Fortunately, I did find a way around this. After a rather long wait on the phone for a private health insurance company (provided by my partner's work), I managed to book an appointment with a well-respected consultant that evening.
More: For people with seasonal affective disorder, winter is literally depressing.
I rushed my afternoon clinic somewhat and was probably not at my best, because I was more worried about myself than most of the patients I saw. I was lucky that a couple of patients did not turn up, so I managed to get to the private hospital just in time and saw a consultant who was reassuring, kind and professional. I had done the right thing to go, but it wasn’t as urgent as I had thought.
A bad case of conscientiousness
I have previously turned up for work on Christmas Eve with a high temperature of 39°C. I realised after a couple of patients that I could see no more, but my thoughts were of the patients who needed to be seen before Christmas and my colleagues, who had done their fair share of working the days nobody wanted to work. After having a rigor (uncontrollable shivers), I drove home leaving a clinic full of patients. In retrospect, whatever possessed me to go to work that day?
Looking after our own health is a problem for GPs. We are notoriously bad at it. We have a sedentary job and lots of stress. We work in small teams and feel incredibly guilty when we need to take time off work to look after ourselves.
I knew that if I had seen a patient with my problem, I would have sent them straight to see a specialist that day.
I do wonder what patients think – they probably would prefer me to cancel the appointment rather than cough all over them. My brain definitely works better and I am a safer doctor when I am well. If I make a mistake when ill, it would not be a defence but a sign that I don’t have insight into being a healthy doctor.
But when could my patients get another appointment? It could be weeks away. They might have arranged their entire day around their appointment. Neither is it fair or safe for my already overworked colleagues to see an extra 30 patients when I am sick.
Learning to look after ourselves
It is also difficult, as a doctor, to treat another doctor. Doctors are tricky patients. They have their own agenda and particular expectations, which may or may not be reasonable. I find that when I am treating doctor patients, I’m a bit anxious and possibly even feeling threatened – the patient might, of course, know more about the subject than me! As they make me feel this way, I probably am not treating them as objectively or as well as I would another patient.
An area we are particularly poor at seeking help with is mental health. It is hard for anyone to admit to feelings of anxiety, depression, or even drug or alcohol misuse, but even harder if we need to confess our feelings to a colleague we might have seen in a meeting that week.
GPs are known to have one of the highest suicide rates of all professions and this is thought partly to be due to the difficulty associated with seeking help from a colleague you might know professionally.
Mental health problems arise because the job is challenging, busy and isolating. We face difficult situations like death and disease daily. We deal with everyone else’s stress and depression, with frequent complaints and with patients’ sometimes unrealistic expectations. Some health professionals have regular psychological support to help them process these issues, but there is nothing set up for GPs.
We need to get better at treating and caring for ourselves. We need an NHS that supports us and values us as employees, and has enough leeway in the system that we aren’t overcome with guilt at letting so many patients down when we take a day off – or week, or however long we need – to look after ourselves.
About the author
The Secret GP
Our anonymous doctor shares what it’s really like behind the scenes in the surgery.
